Key Takeaways from CMS’ PAID Act Testing Webinar

by Frank Fairchok, Vice President of Medicare Reporting Services
Last week, CMS hosted a webinar to discuss the testing plan for changes to the query process. These changes are mandated by the PAID Act, passed on December 11, 2020, giving CMS one year to implement updates to the query process. The law requires CMS to provide enrollment information for beneficiaries for Medicare Part C (Medicare Advantage Plans) and Part D (Prescription Drug Plans). CMS must identify the last three years of enrollment in these plans when responding to the query for identified beneficiaries. While this article will focus on new information related to the testing process that was presented during last Thursday’s webinar, you can find a more in-depth review of the PAID Act here.
UPDATED (9/20): CMS published a copy of the slides from their webinar presentation to the What’s New page on CMS.gov. Below is a summary of the important points from the webinar:
Testing Period
CMS is opening a test period for Responsible Reporting Entities (RREs), and other submitters, starting on September 13, 2021 and ending on December 10, 2021.
During the testing window:
- RREs may submit test files to CMS using the same method they currently use for production files.
- Test files submitted must contain no more than 100 records, as they will be rejected if they exceed that limit.
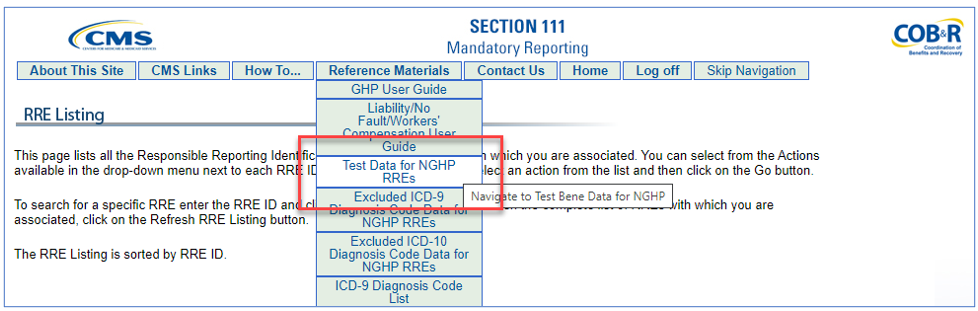
- As shown below, RREs can find files on the Coordination of Benefits Secure Website (COBSW), including test beneficiary data in text and Excel formats and wrapped X12 271 query response file that includes data for the new Part C and D plan fields.
New HEW Software
On September 13, 2021 CMS will release version 5.0 of the HIPAA Eligibility Wrapper (HEW) software, which translates the fixed width text query and query response files into HIPAA-compliant ANSI X12 transaction sets. Version 5.0 will allow side-by-side installation along with the prior version as HEW 4.0 will still be required for production files through December 10, 2021.
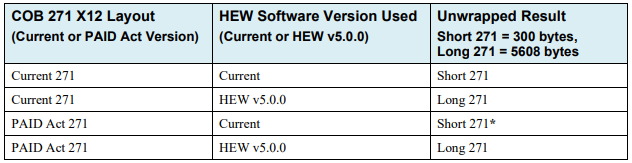
CMS recommends that all RREs submitting files switch to HEW version 5.0 on December 12, 2021. Version 4.0 will still produce a valid query response file after that date, however none of the new data fields will be present and the software will log information-only errors. During the webinar, CMS referred to a table in the NGHP User Guide, version 6.4 in Chapter V, Appendix K as follows:
COBSW Update
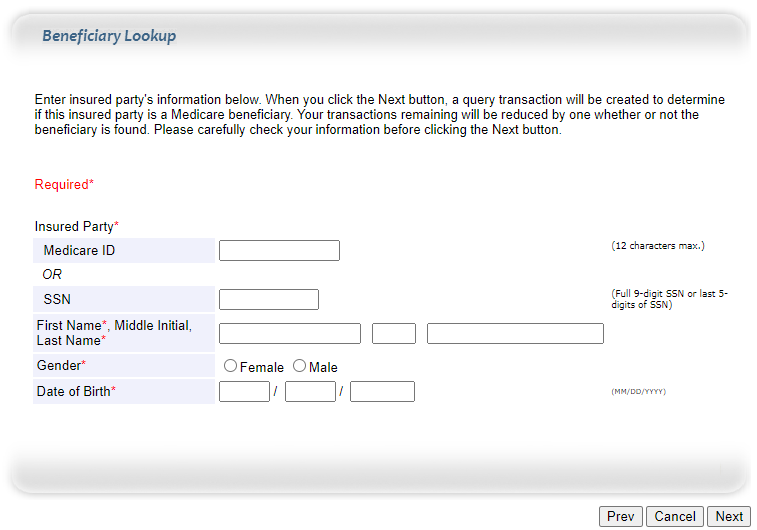
Effective October 4, 2021, CMS will update the Coordination of Benefits Secure Website (COBSW) so that the Beneficiary Lookup function will return three years of Part C and D information, up to 12 instances each. The result screen will also include start and end dates for Parts A and B entitlements. If there are no occurrences of Part C and D enrollment in the past three years, the screen will display the message “No Records Found.”
Question and Answer
CMS answered a variety of questions during the webinar. A summary of some of the more notable points made by CMS in response to questions asked is provided below:
- The Part C and D plan information will start with the most current enrollment date and each subsequent record should be in chronological order.
- HEW 5.0 can be installed alongside version 4.0, but should be installed in a separate directory.
- A copy of the presentation will be published within 7-10 business days from date of webinar.
- Queries submitted prior to December 11, 2021 will receive the 300-byte response, even if the submission is processed on (or after) December 11, 2021.
Commentary
CMS was asked several times about usage of the new data that will be returned in the query response, frequently directed the person asking the question to the mailboxes dedicated to Part C and Part D questions. However, on a slide titled “RREs Choosing Not to Make Changes” the first bullet point stated:
“RREs are not required to use the additional information being provided by the PAID Act.”
While it is true that the PAID Act requires CMS to provide the Part C and D plan information, it does not direct the consumption or usage of that data by Non-Group Health Plan RREs. It is up to each individual RRE to determine if they will use this new information and how they will utilize it. However, these plans have similar rights of recovery as CMS and ignoring the newly available data does not seem likely to strengthen an RREs defense. It is important to note here that “not required to use” the data does not translate into a corresponding lack of responsibility on the part of the RRE to reimburse Medicare and/or the private plans. The technical implementation of the PAID Act is only the beginning of what is sure to be the start of many years of evolution in recovery processes between NGHP RREs and Medicare Advantage and Prescription Drug plans.
MEDVAL is invested in understanding these issues and will monitor the evolution of the PAID Act and its impact on reporting, so we can adapt and continue to meet the needs of our clients.
If you have questions regarding Mandatory Insurer Reporting or the PAID Act, contact us at [email protected].