Key Takeaways from CMS’ PAID Act Webinar

by Frank Fairchok, Vice President of Medicare Reporting Services
Last week, CMS hosted a webinar to discuss upcoming changes to Section 111 Reporting for Non-Group Health Plan entities. These changes are related to the PAID Act, which was signed into law on December 11, 2020 giving CMS one year to begin providing Medicare Part C and Part D enrollment information in the query response file. The intent of these changes is to allow Responsible Reporting Entities (RREs) to better coordinate benefits and recovery processes for a beneficiary/claimant who has been enrolled in a Part C or Part D plan during the preceding three-year period.
Highlights of the CMS Presentation
CMS kicked off the webinar with an overview of the Medicare Secondary Payer Act and the PAID Act. When providing background on the PAID Act, CMS acknowledged once again that
“Non-Group Health plan (NGHP) Responsible Reporting Entities (RREs) did not have a reliable way to identify if a beneficiary had a Part C or Part D plan.” With that statement, CMS provided the following estimates around Part C and D plans:
- 1 in 3 beneficiaries are enrolled in a Part C plan
- 9 in 10 beneficiaries are enrolled in a Part D plan
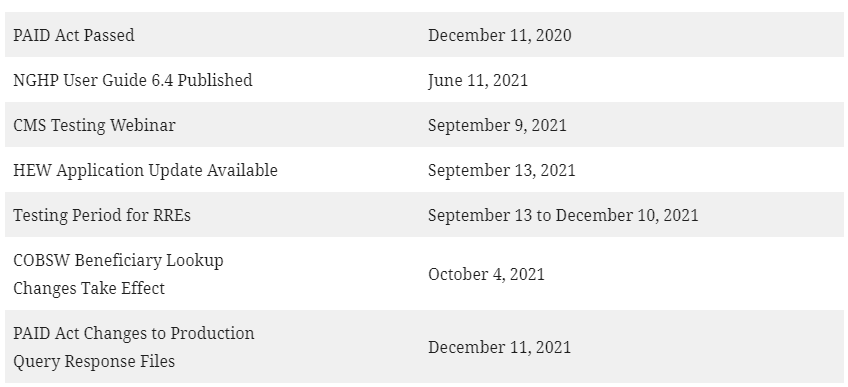
CMS then presented information around query response file changes, testing plans, and COBSW updates. They also provided a calendar of important dates before launching a question and answer session.
UPDATED (7/7): CMS published a copy of the slides from their webinar presentation to the What’s New page on CMS.gov. Below is a summary of the important points from the webinar:
Query Response File Changes
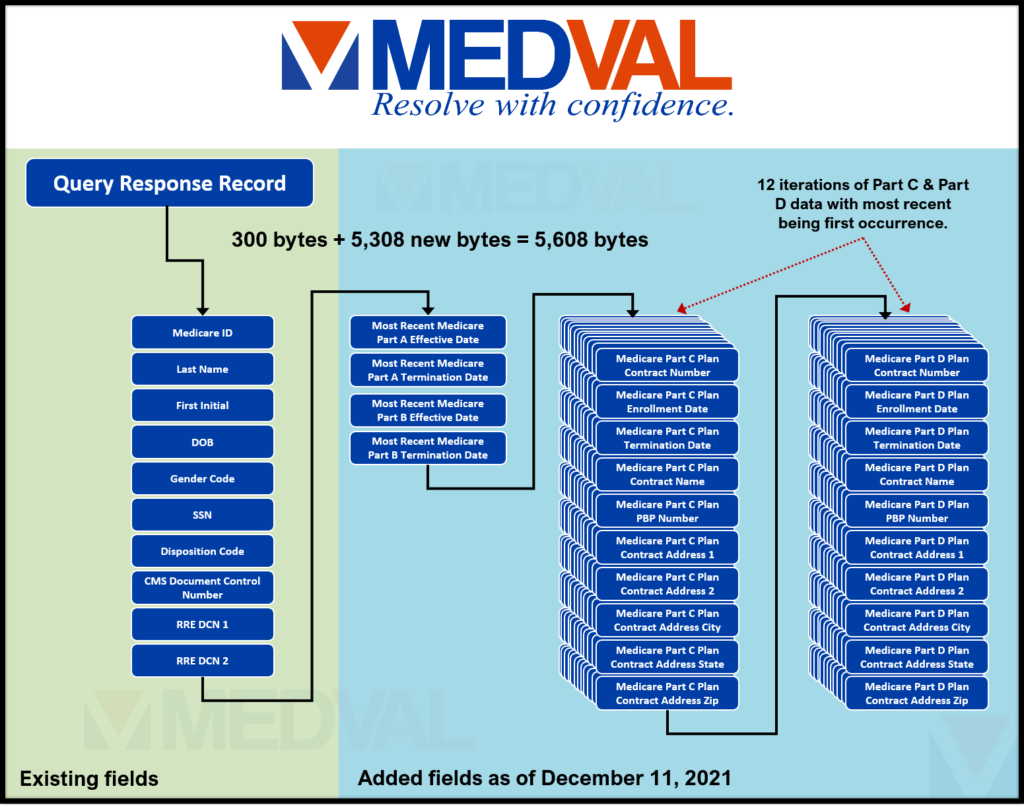
The query response file will increase in size from 300 characters to 5,608 on December 11, 2021. The new format will add enrollment and termination dates for Parts A and B coverage along with 12 iterations each of Parts C and D coverage. Information provided for Parts C and D coverage will include a history going back three years from the date of query, up to twelve instances, and will contain plan contract identifiers, address information, and enrollment dates. MEDVAL has provided a graphic reflecting these changes below, but readers can find the full technical specifications in Table E-4 of Chapter V: Appendices of the NGHP User Guide Version 6.4.
Testing Plan
To transition from the old query response format to the new one, CMS is providing a testing period starting on September 13, 2021 and ending on December 10, 2021. Testing with CMS is encouraged but not required. CMS will be hosting a webinar specific to testing on September 9, 2021 and will be providing more information about the webinar soon. We would like to remind readers that while the new file goes into production on December 11, 2021 – there is no backward compatibility. As such, any entity with a need to read the query response file will need to adapt to these specification changes, as well as install the HIPAA Eligibility Wrapper (HEW) software update provided by CMS before the testing period begins.
COBSW Updates
In conjunction with making file layout changes, CMS is updating the Coordination of Benefits Secure Website (COBSW). The COBSW site currently allows an RRE’s Account Manager or Account Designee(s) to manually query up to 500 records per calendar month. Starting on October 4, 2021, CMS will update the information being returned to include the new PAID Act data fields
Calendar of Dates
CMS provided the following list of dates related to changes stemming from the PAID Act:
Question and Answer
CMS spent most of the webinar answering questions from the audience. A summary of some of the more notable points made by CMS in the response to questions received is provided below:
- A transcript of the webinar will be available in 7-10 days from the date of the webinar.
- The 12 instances of Part C and Part D information will be restricted to the three years prior to the query date.
- Limited Section 111 reporting data is shared with Part C and D plan providers. While the data shared includes a view to the primary payer, ORM or TPOC data is not provided.
- No changes to the Section 111 reporting process are being made with the PAID Act updates, nor are there changes to the recovery processes for Part C and D plans.
Several questions asked sought to determine if receiving this new information around historical Part C and D plans presented the RRE with an obligation to use the data to track down recovery cases with the plans. CMS did not directly answer these questions, but rather stated that no changes were being made to the plans’ processes from a CMS perspective.
Commentary
While the new Part C and D plan data may not present an obligation to the RRE to use the data to identify potential recovery issues, it clearly presents an opportunity to identify those issues and resolve them prior to settlement. There are many questions still unanswered and there are sure to be a variety of developments as we move forward. For example:
- Does the knowledge of the Part C and D plan data on behalf of the RRE, or the knowledge of a primary payer on behalf of the plans strengthen or weaken recovery cases?
- How long can a Part C or D plan take to respond once an RRE, or its recovery agent, has inquired about their interest in a claim?
- Will time taken by these plans to respond have an impact on how quickly a claim can be settled?
- Will any part of this process have an impact on the MSP Private Cause of Action cases?
MEDVAL is invested in understanding these issues and will monitor the evolution of the PAID Act and its impact on reporting, so we can adapt and continue to meet the needs of our clients.
If you have questions regarding Mandatory Insurer Reporting or the PAID Act, contact us at [email protected].